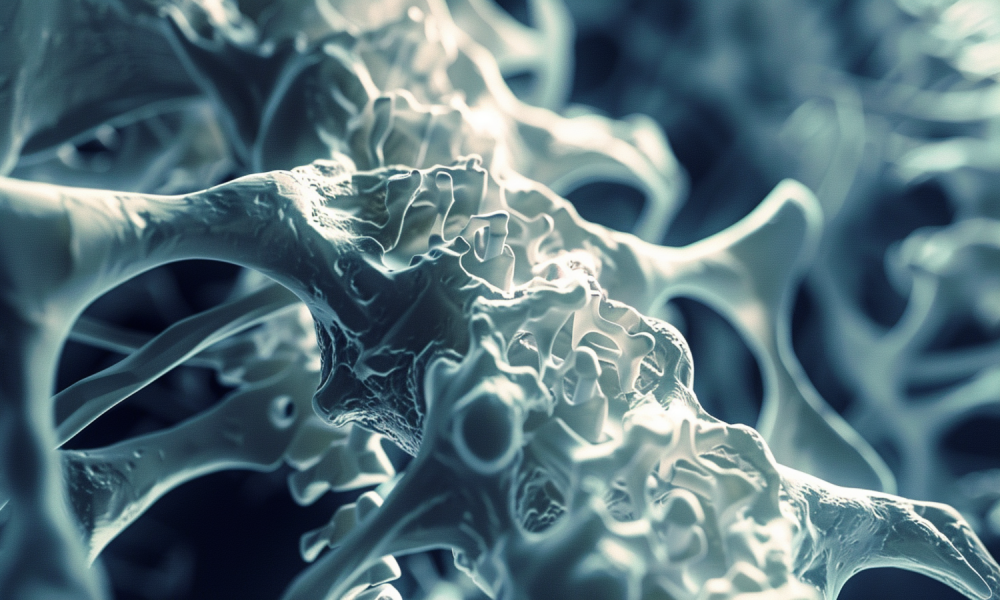
Osteoporosis, the silent thief, has been elusive for too long. This bone thief often goes undetected until a fracture occurs. But now AI is poised to unmask osteoporosis” silent cues before they become a breaking point.
It’s not as if we do not have the means to test for osteoporosis because we have, and it is known as dual-energy X-ray absorptiometry (DXA). It is the current gold standard for measuring bone mineral density (BMD). However, it has limitations.
DXA scans require specialized equipment and personnel, making them inaccessible and expensive. As a result, many at-risk individuals remain unscreened until they experience a fracture.
With AI in the scene, this will soon change. Recent breakthroughs show that AI algorithms, especially deep learning models, can accurately predict osteoporosis risk using existing health data. This could mean earlier detection and intervention, potentially no fractures, and better outcomes.
Moreover, pioneering research from Tulane University confirms the potential of artificial intelligence in osteoporosis detection. Scientists there developed a deep neural network (DNN) model specifically designed to predict the risk of osteoporosis.
This model was rigorously tested against traditional machine learning algorithms and a conventional regression model. They utilized data from over 8,000 participants enrolled in the Louisiana Osteoporosis Study, demonstrating the DNN model’s advanced capabilities in accurately assessing osteoporosis risk.
The DNN model performed better than the competition in predicting osteoporosis risk. It was good at identifying high-risk individuals (sensitivity) and low-risk individuals (specificity).
The model suggests that AI can be used for osteoporosis screening using existing health data and expanding access to screening, especially where DXA is not available. Notably, the DNN model identified these top 10 osteoporosis risk factors:
- Weight
- Age
- Gender
- Grip strength
- Height
- Beer consumption
- Diastolic blood pressure
- Alcohol intake
- Smoking duration
- Income level
Current osteoporosis screening guidelines, on the other hand, rely heavily on age and gender. While important, these factors don’t really capture an individual’s unique risk profile. However, AI offers a more personalized approach.
By considering a wide range of factors, including modifiable lifestyle choices like smoking and alcohol use, AI can identify high-risk individuals who may slip through the cracks of current screening protocols. This targeted approach could revolutionize prevention strategies.
Individuals identified by AI as high-risk can undergo DXA scans to confirm the diagnosis and then begin bone-strengthening medications and lifestyle adjustments. Additionally, they can receive more frequent monitoring for signs of fractures.
On a societal level, AI-driven risk stratification can optimize resource allocation. For instance, DXA and advanced testing can be prioritized for the highest-risk individuals, and low-risk individuals can avoid unnecessary testing and treatment.
However, the path to widespread AI implementation in osteoporosis screening is fraught with challenges. The Tulane study requires validation in diverse populations and real-world clinical settings. Additionally, ethical and legal hurdles, including model fairness, patient privacy, and liability, must be addressed. Let’s look at some of these challenges:
Data Bias
AI models can only be as unbiased as their training data. If the data does not represent the general population, the model’s predictions will not be universally applicable. We need strong safeguards to prevent AI from exacerbating health disparities.
Patient Privacy
Training AI models requires access to large health data repositories, but this data must be protected. Patients must trust that their sensitive health information will be private and secure.
Liability
If an AI model fails to identify a high-risk individual who later suffers a fracture, who is held responsible? The AI developers? The healthcare providers who relied on its predictions? Hence, as AI becomes increasingly prevalent in medicine, legal and regulatory frameworks must evolve to provide clear guidelines.
But despite the challenges, AI is no doubt quite exciting to the medical community. Why won’t it be? After all, if AI can identify at-risk individuals earlier, it can change the outcome for millions of people worldwide.
Statistically speaking, every three seconds, an osteoporotic fracture occurs globally. These fractures, especially of the hip, can trigger a cascade of consequences, including:
- Chronic pain
- Disability
- Loss of independence
- Increased mortality
On the economic front, too, the impact is significant, with osteoporosis-related fractures costing billions annually in healthcare expenses and lost productivity.
The only way to nip these problems in the bud is through early detection and treatment. Only then can we prevent these fractures. Research indicates that bone-strengthening medications like bisphosphonates can significantly reduce fracture risk in osteoporosis patients. However, these medications are underused, partly because osteoporosis often goes undiagnosed.
Beyond Just Diagnosis
Personalization
AI models can predict how individuals will respond to treatments, enabling personalized therapy choices. They can also monitor treatment adherence and effectiveness over time, alerting healthcare providers when adjustments are necessary.
Looking ahead, AI could even be integrated into consumer health devices. Imagine a smartwatch that tracks your activity, diet, and other health metrics, providing personalized osteoporosis risk assessments and preventive advice. Such a device would empower you to manage your bone health and overall health proactively. However, achieving this requires collaboration among AI researchers, healthcare providers, and patients.
Affordable Early Osteoporosis Detection
Next comes the affordability aspect, highlighting the beauty of AI in democratizing early osteoporosis detection. While DXA scans are effective, they are neither practical nor affordable on a population scale. The solution lies in a validated AI algorithm that can be deployed through electronic health record systems. This is particularly beneficial in underserved communities where osteoporosis often goes undiagnosed, making early detection more accessible and affordable for all.
Better Accessibility & Utilization
Moreover, rural areas with limited access to specialists and DXA could utilize AI to identify high-risk patients for referral. Older adults with mobility issues could be screened without needing to travel for a scan. Additionally, AI-generated risk scores could help prioritize DXA resources for those who would benefit the most, ensuring that the available resources are used efficiently and effectively.
Instead of relying on broad screening guidelines based on age or gender, AI could enable targeted screening based on individual risk profiles, optimizing patient outcomes and resource utilization. Beyond early detection, AI could improve osteoporosis management by predicting patient trajectories and enabling personalized interventions.
Now, let’s look at companies that could benefit from advancements in AI-driven osteoporosis detection and management.
#1. Hologic, Inc. (HOLX)
Hologix is a leading provider of DXA systems used to measure bone density. By integrating AI into their DXA systems, Hologic can significantly enhance the accuracy and predictive capabilities of osteoporosis detection.
This improvement can make their products more valuable and attractive to healthcare providers, potentially increasing sales of their DXA systems and associated software, thereby expanding their market share in osteoporosis diagnostics.
Financially, the company is in a solid position. It reported a total revenue of approximately $4.03 billion for the fiscal year 2023.
#2. GE Healthcare
As a major player in medical imaging, GE Healthcare can benefit from AI advancements by enhancing the diagnostic capabilities of its imaging systems, including DXA scanners.
Improved AI integration can result in more precise and early detection of osteoporosis, driving demand for their advanced imaging technologies and AI software solutions. This can lead to higher sales and long-term service agreements, strengthening their position in the medical imaging market.
Revenue-wise, GE Healthcare reported a total revenue of $19.6 billion for the fiscal year 2023.
Concluding Thoughts
Overall, although these developments and potential benefits sound incredible, they are unlikely to happen overnight. Ongoing research, development, validation, and addressing the challenges around data privacy, security, ethics, and equity are essential. However, if we get it right, the rewards will be immense. We can transform this silent disease into one that is preventable, treatable, and ultimately defeatable.
Click here to learn all about investing in artificial intelligence.